Health
Why Screening Visits Often Cost Less Than Tests Done for Symptoms

Most people have had that uneasy moment when they see a medical bill that seems higher than expected. It often raises a question: why do some tests cost more than others, even when they look almost the same? This difference is especially noticeable when comparing preventive screenings to tests ordered after symptoms appear.
Understanding how pricing works in healthcare can be confusing. Preventive screenings such as a routine colonoscopy or mammogram may have lower out-of-pocket costs, while the same test done because of a symptom might be billed differently. The reason lies in how insurance plans classify care and how medical visits are coded and reimbursed.
Knowing what makes screenings less expensive can help people make informed health choices and avoid surprising costs. For example, learning about the colonoscopy screening price compared to one done to check a medical concern can highlight how preventive care can actually save money in the long run.
Insurance Incentives for Preventive Care
Modern healthcare systems encourage people to stay healthy before problems start. Insurance plans often reflect this goal, rewarding preventive care with lower costs or full coverage.
Covered Under Preventive Benefits
When a service is labeled as preventive, most insurance plans must cover it fully under national healthcare guidelines. That means no deductible, copay, or coinsurance for eligible screenings. For example, when someone gets a routine screening test at the recommended age, their health plan usually pays the full amount.
This structure is meant to remove financial barriers so people don’t skip care that could catch disease early. It’s a financial nudge toward prevention—and a major reason screening visits often cost less than the same tests ordered later for a medical concern.
The Purpose of the Visit Matters
Pricing differences don’t happen by accident. The reason for the visit plays a major role in how billing codes are assigned. A screening code signals prevention, while a diagnostic code flags that a symptom or prior finding prompted the test. Once a visit shifts from preventive to diagnostic, the cost responsibilities often change.
For instance, if a doctor orders a test because someone reported abdominal pain, it’s no longer preventive under insurance rules. Even if the test looks identical to a screening one, the coding triggers different billing—and usually a patient payment. Understanding this small detail can help patients ask the right questions before their visit.
Long-Term Savings Through Early Detection
Preventive screening is not only covered differently but also saves money in the long run. Detecting problems before they become serious often prevents expensive treatments later. When diseases like cancer or heart disease are caught early, the cost—and emotional toll—of care can be far lower.
Health systems and insurers know this, which is why they structure plans to encourage screenings. It costs less to remove a small growth during a screening visit than to treat an advanced condition later. Prevention is both smart medicine and sound financial planning.
Diagnostic Visits Involve More Complexity
Tests ordered for symptoms typically cost more because they require more resources and deeper investigation. From specialist consultations to additional testing, diagnostic care often turns into a longer, more complicated process.
More Steps and Specialized Care
A diagnostic visit begins when someone reports a symptom—pain, unexplained bleeding, or another change. The doctor’s job then becomes figuring out the cause. This often leads to additional imaging, lab tests, or follow-up visits. Each adds cost.
Diagnostic care may also involve specialists working together, which can increase overall expenses. The time, expertise, and coordination needed for accurate diagnosis are naturally more involved than a routine checkup. That complexity is reflected in how the healthcare system prices these visits.
Insurance Cost Division for Diagnostic Care
Unlike preventive services, diagnostic tests usually fall under the patient’s cost-sharing plan. That means deductibles, copays, or coinsurance may apply. For example, if a person undergoes a colonoscopy after reporting symptoms, the visit is reclassified from preventive to diagnostic care. Even though the procedure is identical, the out-of-pocket cost may rise significantly because the purpose changed.
This difference can surprise patients, but it’s rooted in how insurance contracts are structured. Insurers view diagnostic testing as a service tied to treatment rather than prevention, shifting part of the expense to the patient.
How Understanding Costs Can Guide Better Choices
Knowing why preventive screenings cost less helps people plan their care more confidently. It encourages scheduling recommended screenings before symptoms appear and clarifying visit details ahead of time.
Asking the Right Questions Before a Visit
Patients can better manage costs by confirming how their visit will be billed before getting tested. Asking questions such as “Is this coded as a preventive screening?” or “Will this count as diagnostic under my plan?” can make a significant difference in what someone pays.
Medical offices handle billing daily and can explain what classification applies based on the reason for the test. A brief conversation beforehand can help prevent confusion when the bill arrives.
The Value of Preventive Care Awareness
Making preventive care a habit does more than reduce medical bills. It helps people stay aware of their health, build trust with their doctor, and address potential problems early. When screenings are done at the recommended times, the benefit extends beyond financial savings—it supports peace of mind and long-term well-being.
Understanding the cost difference also encourages people to act before symptoms appear, rather than waiting until something feels wrong. That awareness can be life-saving, especially with preventive exams that detect silent conditions.
Choosing Prevention for Better Health
In healthcare, timing matters—not only for treatment but also for cost. A test done proactively as part of a screening visit is often less expensive than the same test performed because of symptoms. The difference comes down to insurance coverage, coding practices, and the broader goal of promoting prevention.
Recognizing these cost distinctions helps people make smarter health decisions. Whether it’s understanding the typical colonoscopy screening price or confirming coverage for an annual exam, small steps toward awareness can lead to big savings and healthier outcomes. Preventive care remains one of the simplest ways to protect both well-being and the wallet.
For More Information Visit Coopermagazine
-

 Celebrity1 year ago
Celebrity1 year agoWho Is Jennifer Rauchet?: All You Need To Know About Pete Hegseth’s Wife
-

 Celebrity1 year ago
Celebrity1 year agoWho Is Mindy Jennings?: All You Need To Know About Ken Jennings Wife
-
 Celebrity1 year ago
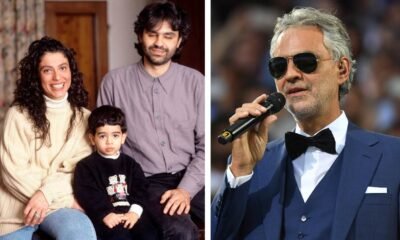
Celebrity1 year agoWho Is Enrica Cenzatti?: The Untold Story of Andrea Bocelli’s Ex-Wife
-

 Celebrity1 year ago
Celebrity1 year agoWho Is Klarissa Munz: The Untold Story of Freddie Highmore’s Wife
















