Health
6 Ways To Manage Blood Sugar And Support Long-Term Weight Goals

Keeping blood sugar steady day to day does more than prevent dips and spikes. It supports the habits that make weight goals stick. Use these science-backed moves and build a routine you can carry for years.
Lift Weights For Insulin Sensitivity
Resistance training helps your muscles soak up glucose more efficiently and supports weight management when done consistently.
A 2025 meta-analysis in a leading endocrinology journal reported that resistance exercise showed notable benefits for improving insulin sensitivity across randomized trials. Aim for 2 to 3 short sessions per week, focusing on big moves like squats, rows, and presses.
Start with loads that allow clean form and leave one or two reps in reserve. Rest days matter since insulin sensitivity gains compound as muscles recover and adapt. If time is tight, full-body circuits can deliver results in 20 to 30 minutes.
Pair lifting days with adequate protein to support muscle repair and satiety. Consistency over months matters far more than chasing heavy numbers early.
Think About Medication As One Tool
Medication can be part of a broader plan that includes nutrition, movement, and sleep. For some people, a Liraglutide Prescription can help regulate appetite and improve glucose control – talk with your clinician about fit, dosing, and how it pairs with your daily routine. It is still important to keep up the basics like protein at meals and regular activity.
Medication works best when expectations are realistic, and progress is reviewed regularly. Track how hunger, energy, and side effects change week to week so adjustments are based on patterns, not single days.
Set small behavior goals alongside the prescription, such as consistent meal timing or short walks after eating.
Plan for plateaus and discuss them early rather than stopping abruptly out of frustration. Seen this way, medication supports habits instead of replacing them.
Add Short Cardio Bursts After Meals
You do not need an hour on the treadmill to make a dent in post-meal glucose. Try 10 to 15 minutes of brisk walking, cycling, or stair climbing within 30 to 60 minutes after eating. These mini sessions can reduce the size of your glucose rise and make it easier to stay on track with calories later.
Keep the effort moderate so it feels sustainable, not punishing. You should be able to talk in short phrases without gasping for air.
Consistency matters more than intensity on busy days. Pair the habit with something you already do, like a phone call or podcast, to make it automatic. These short bursts add up to meaningful metabolic benefits.
Use CGM Feedback To Shape Habits
Feedback loops matter when you are building new routines. Recent clinical guidance noted growing consideration of continuous glucose monitoring for some adults with type 2 diabetes who are not on insulin, highlighting its potential beyond just numbers.
If you use a CGM under medical guidance, review patterns weekly and pick one small behavior to test based on what you see.
- Choose one change at a time
- Test it for 1 to 2 weeks
- Recheck your pattern and adjust
Focus on trends rather than single spikes, so the data stays useful instead of stressful. Pair readings with brief notes about meals, sleep, and stress to give context to the graph. Look for repeatable wins, like a short walk that consistently smooths post-meal rises.
Share summaries with your clinician to align experiments with your plan. Treat the CGM as a coach for habits, not a judge of daily perfection.
Match Treatment To Heart And Metabolic Risk
Your plan should reflect more than glucose alone.
Expert guidance in a prominent diabetes journal highlighted that for adults with type 2 diabetes who have or are at high risk for cardiovascular disease, a GLP-1 receptor agonist and or an SGLT2 inhibitor should be considered to reduce events.
Ask about how options align with your history, side effects, and insurance coverage. This approach helps avoid treating numbers in isolation and missing bigger risks. Cardiovascular history, kidney function, weight goals, and tolerance all shape which therapy fits best.
Some medications offer added benefits like modest weight loss or blood pressure improvements, which can matter long term.
Others may require closer monitoring or lifestyle adjustments to manage side effects. A shared decision conversation keeps treatment realistic and sustainable instead of reactive.

Build Meals That Blunt Spikes
Use a simple plate plan: protein, fiber-rich carbs, and some healthy fat. Start with nonstarchy vegetables, add a palm-sized portion of protein, then fill the rest with beans, lentils, whole grains, or fruit.
Keep sweetened drinks and refined snacks for rare occasions, and eat them with a meal rather than alone.
When your habits line up with your goals, weight loss and stable glucose become easier to maintain. Start with one strength session and one post-meal walk this week – small steps stack up fast.
-

 Celebrity1 year ago
Celebrity1 year agoWho Is Jennifer Rauchet?: All You Need To Know About Pete Hegseth’s Wife
-

 Celebrity1 year ago
Celebrity1 year agoWho Is Mindy Jennings?: All You Need To Know About Ken Jennings Wife
-
 Celebrity1 year ago
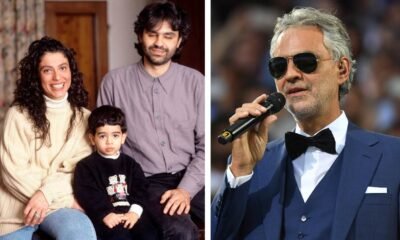
Celebrity1 year agoWho Is Enrica Cenzatti?: The Untold Story of Andrea Bocelli’s Ex-Wife
-

 Celebrity1 year ago
Celebrity1 year agoWho Is Klarissa Munz: The Untold Story of Freddie Highmore’s Wife
















